[ad_1]
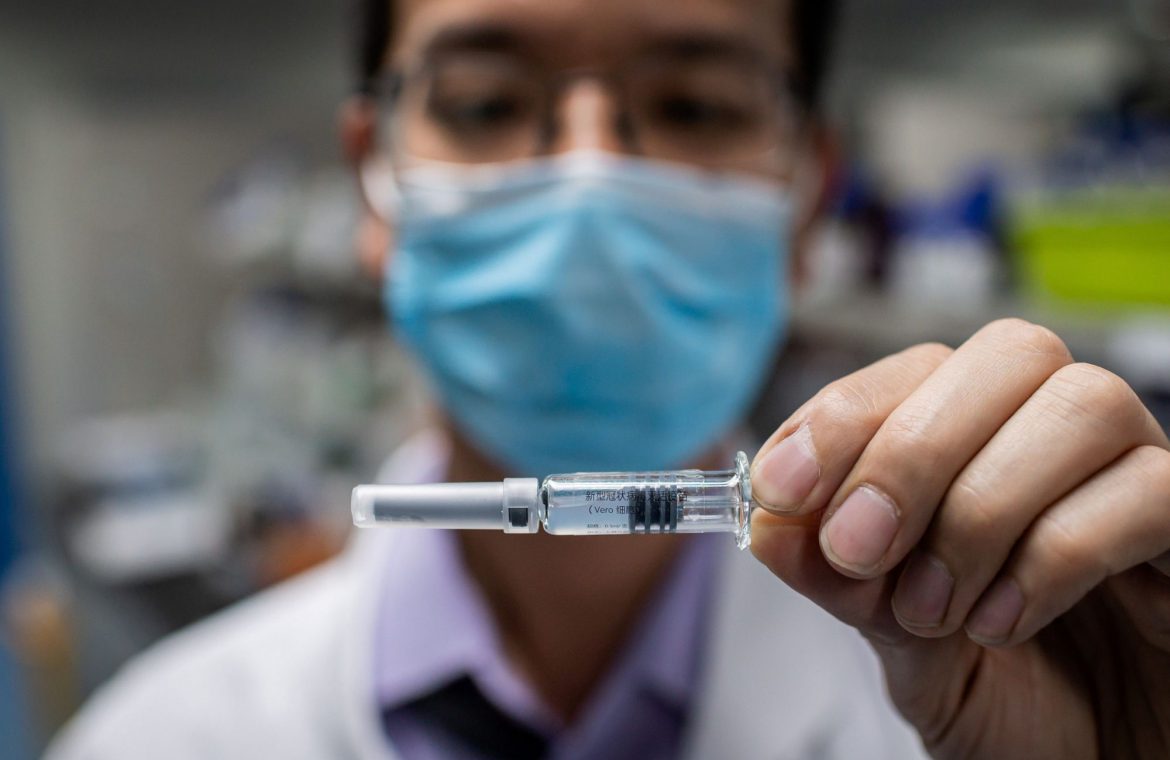
A 16-year-old in Pfizer’s clinical trial to test its coronavirus vaccine candidate. She was the first adolescent patient at Cincinnati Children’s Hospital to enroll in the study. Cincinnati Children’s Hospital
We just took a big step forward in confronting the coronavirus pandemic.
Pfizer on Monday said its coronavirus vaccine was found to be highly effective at preventing COVID-19, the disease caused by the novel coronavirus. The findings come from a massive and well-designed study, but they haven’t been reviewed by outside experts or by regulators.
The news of a successful vaccine sent markets soaring with the hope that it could end the pandemic.
But there’s a lot to keep in mind about what the results mean for the pandemic and for when Americans might be able to get a shot.
Here’s what you need to know.
1. Don’t expect to get a vaccine just yet
Pfizer on Monday described the first results from its 43,538-person trial in a press release. The trial is ongoing, so these are interim results taken after 94 people in the trial got infected with COVID-19.
It’s the first of many steps in getting the vaccine to Americans. Later in November, once it’s able to provide more information about how safe the vaccine is, the drugmaker plans to apply for an emergency use authorization from the Food and Drug Administration.
Then FDA experts and outside scientists will review the data before deciding whether the vaccine can be given to people more widely.
The Centers for Disease Control and Prevention has estimated that the US will have a supply of about 20 million to 30 million doses of Pfizer’s vaccine in 2020, translating to enough doses to vaccinate less than 10% of the population.
Story continues
Government officials have said it’ll take until mid-2021 to get a widely available vaccine. Higher-risk populations, such as older people and healthcare workers, are likely to get the shots first.
2. Rolling out hundreds of millions of vaccine doses presents a logistical nightmare
Should the FDA authorize Pfizer’s vaccine, it’ll take some time to ramp up and distribute the hundreds of millions of doses needed to vaccinate the US population. And it’ll pose some unusual logistical challenges along the way.
The vaccine needs to be shipped and stored at negative 94 degrees Fahrenheit, a temperature colder than what’s needed to store most other vaccines. That will be challenging in the US and present even more of an obstacle in some other countries.
“The onerous freezer chain requirements will certainly be a challenge not only here in the US but globally,” Maria Elena Bottazzi, a codirector of Texas Children’s Hospital Center for Vaccine Development and associate dean of Baylor College of Medicine’s National School of Tropical Medicine, said in an email on Monday.
Getty3. Vaccine rivals still expect results in 2020
Pfizer’s positive results should be a good sign for other vaccine frontrunners like Moderna, AstraZeneca, and Johnson & Johnson, which are racing to prove that their shots are also effective in preventing COVID-19.
Pfizer and BioNTech developed a messenger-RNA vaccine, which requires just the genetic code of the virus to engineer an experimental vaccine.
Pfizer’s result on Monday was the first to indicate that the technology works in humans. Moderna, which also specializes in mRNA therapeutics and vaccines, was the world’s first drugmaker to start testing a COVID-19 vaccine in humans in March.
The first successful results should also validate the target that all the frontrunners are going after. All these shots target the same portion of the coronavirus: its spike protein.
4. The US will foot the bill for the vaccines
The US government’s coronavirus-vaccine initiative, Operation Warp Speed, secured 100 million doses in July through a $1.95 billion deal with Pfizer.
That agreement should make the vaccine free for all Americans. In late October, the government rolled out details about preventing out-of-pocket costs to receive the vaccine, including waiving deductibles and copays for people on Medicare and requiring most private health-insurance plans to cover the vaccine without any cost-sharing.
5. We don’t yet know whether vaccinated people could be asymptomatic carriers
Questions remain about this vaccine, as a single study can’t address every concern about the shot.
Real-world use across millions of people will be the only way to learn exactly how protective the shots are and whether there are any rare but serious side effects.
For instance, the study didn’t regularly test volunteers to see whether the shots prevented asymptomatic infection; volunteers were tested for the virus only if they reported symptoms.
That means vaccinated people could still be infectious and contagious. It’s unclear how well the vaccine prevents people from becoming asymptomatic carriers — if it does at all.
The early results also don’t tell us whether the vaccine protects against both mild and severe illness, Bottazzi told Business Insider.
Pfizer’s study looked at whether the vaccine reduced symptomatic COVID-19 cases, regardless of the severity of the symptoms. Some experts want to see data on whether the vaccine also reduces hospitalization and death rates.
It’ll be some time before the trial concludes and we know exactly how well the vaccine works. While Pfizer said the initial analysis found that the vaccine was more than 90% effective, that percentage might change as we get more data on trial participants who’ve gotten infected with COVID-19.
6. Don’t throw your mask away just yet
Simply having a coronavirus vaccine may not let us get back to normal immediately.
Even if some people receive a safe and effective vaccine next year, that doesn’t mean people will be able to stop wearing masks and social distancing, researchers told Business Insider.
It’ll largely come down to how effective the vaccines are — making Pfizer’s announcement that its vaccine is more than 90% effective promising.
Vaccines have different levels of effectiveness. An ideal shot provides what vaccine developers call sterilizing immunity, which reliably protects people from getting infected. Many vaccines don’t meet this bar. These shots can lower the chance of developing symptoms of a disease, even if some people still get infected.
Read more: Even if there’s a coronavirus vaccine next year, don’t expect to throw away your mask and stop social distancing, a top vaccine developer says
7. Finding an effective vaccine in less than a year is a massive feat
In all, Pfizer’s announcement on Monday is a momentous breakthrough in the world’s battle with this virus.
Developing and testing an effective vaccine in less than a year is an unprecedented accomplishment in medicine.
And having a vaccine distributed in 2021 should give society the upper hand on the virus, which has infected 9.5 million people in the US and killed about 227,000 people.
As of November, daily new cases in the US had surged to more than 116,000. And hospitals around the country are at risk of becoming overwhelmed.
Read the original article on Business Insider
[ad_2]
Source link